RESEARCH ARTICLE
Agrammatism and Paragrammatism: A Cortical
Double Dissociation Revealed by
Lesion-Symptom Mapping
a n o p e n a c c e s s
j o u r n a l
Julius Fridriksson2, and Gregory Hickok4
William Matchin1
, Alexandra Basilakos2
, Brielle C. Stark3
, Dirk-Bart den Ouden2
,
1University of South Carolina
2Department of Communication Sciences and Disorders, University of South Carolina
3ISpeech and Hearing Sciences Department and Program in Neuroscience Faculty, Indiana University Bloomington
4Department of Cognitive Sciences, Department of Language Sciences, University of California, Irvine
Keywords: aphasia, agrammatism, paragrammatism, syntax, fluency, lesion-symptom mapping
ABSTRACT
The fundamental distinction of grammatical deficits in aphasia, agrammatism and
paragrammatism, was made over a century ago. However, the extent to which the
agrammatism/paragrammatism distinction exists independently of differences in speech
fluency has not clearly been investigated. Despite much research on agrammatism, the lesion
correlates of paragrammatism are essentially unknown. Lesion-symptom mapping was used to
investigate the degree to which the lesion correlates of agrammatism and paragrammatism
overlap or dissociate. Four expert raters assessed videos of 53 right-handed patients with
aphasia following chronic left-hemisphere stroke retelling the Cinderella story. Consensus
discussion determined each subject’s classification with respect to grammatical deficits as
Agrammatic, Paragrammatic, Both, or No Grammatical Deficit. Each subject’s lesion was
manually drawn on a high-resolution MRI and warped to standard space for group analyses.
Lesion-symptom mapping analyses were performed in NiiStat including lesion volume as a
covariate. Secondary analyses included speech rate (words per minute) as an additional
covariate. Region of interest analyses identified a double dissociation between these
syndromes: damage to Broca’s area was significantly associated with agrammatism, p = 0.001
(but not paragrammatism, p = 0.930), while damage to the left posterior superior and middle
temporal gyri was significantly associated with paragrammatism, p < 0.001 (but not
agrammatism, p = 0.873). The same results obtained when regressing out the effect of speech
rate, and nonoverlapping lesion distributions between the syndromes were confirmed by
uncorrected whole brain analyses. Our results support a fundamental distinction between
agrammatism and paragrammatism.
INTRODUCTION
Kleist (1914) noted two kinds of syntactic disturbances in the speech of patients with aphasia:
agrammatism and paragrammatism. Agrammatism is described as the simplification of gram-
matical structure and omission of function words and morphemes. For example, Goodglass
(1993) reports this example of agrammatic speech:
Examiner: What brought you to the hospital?
Patient: Yeah…Wednesday, …Paul and dad…Hospital…yeah…doctors, two…an’ teeth.
Citation: Matchin, W., Basilakos, A.,
Stark, B. C., den Ouden, D.-B.,
Fridriksson, J., & Hickok, G. (2020).
Agrammatism and paragrammatism: A
cortical double dissociation revealed
by lesion-symptom mapping.
Neurobiology of Language, 1(2),
208–225. https://doi.org/10.1162/
nol_a_00010
DOI:
https://doi.org/10.1162/nol_a_00010
Supporting Information:
https://doi.org/10.1162/nol_a_00010
Received: 15 January 2020
Accepted: 27 March 2020
Competing Interests: The authors have
declared that no competing interests
exist.
Corresponding Author:
William Matchin
matchin@mailbox.sc.edu
Handling Editor:
Kate Watkins
Copyright: © 2020 Massachusetts
Institute of Technology. Published
under a Creative Commons Attribution
4.0 International (CC BY 4.0) license.
The MIT Press
l
D
o
w
n
o
a
d
e
d
f
r
o
m
h
t
t
p
:
/
/
d
i
r
e
c
t
.
m
i
t
.
e
d
u
n
o
/
l
/
l
a
r
t
i
c
e
-
p
d
f
/
/
/
/
1
2
2
0
8
1
8
6
7
6
9
6
n
o
_
a
_
0
0
0
1
0
p
d
.
/
l
f
b
y
g
u
e
s
t
t
o
n
0
7
S
e
p
e
m
b
e
r
2
0
2
3
Agrammatism and paragrammatism
Paragrammatism:
common symptom of fluent aphasia.
Syntactic errors are not attributable to
overall simplification or omission of
functional elements (e.g., agreement
errors).
Agrammatism:
common symptom of nonfluent
aphasia. Syntax is simplified and
function words and morphemes
(e.g., articles, past tense) are
omitted.
Fluency:
ease of production, particularly
applied to aphasia. Includes both
quantity and quality of speech.
Nonfluent aphasia:
aphasias characterized by typically
nonfluent production, including
Broca’s aphasia, global aphasia,
and anomia.
Fluent aphasia:
aphasias characterized by typically
fluent production, including
Wernicke’s aphasia, conduction
aphasia, and anomia.
Lesion-symptom mapping:
method of determining the
relationship between the extent and
location of brain damage with
behavioral measures or deficits.
Syntax:
sentence structure. Includes both
linear information (e.g., word order)
and hierarchical information
(grouping of words into phrases).
Morphosyntax:
internal structure of words and
sentences. Includes syntactic features
marked on words (e.g., plural -s,
past tense -ed).
Paragrammatism, by contrast, is the misuse of grammar not attributable to an overall
reduction of grammatical morphemes or simplification of syntactic structure. Kleist (1914)
noted the prodigious output of paragrammatic patients, leading to “confused sentence
monsters.” Butterworth and Howard (1987) provide examples of paragrammatic speech:
“And I want everything to be so talk.” (p. 13)
“She was handled to look at the books a bit.” (p. 14)
“I’m very want it.” (p. 19)
“Isn’t look very dear, is it?” (p. 19)
“But it’s silly, aren’t they?” (p. 20)
Agrammatism has received extensive treatment in the literature and is widely known by
both researchers and clinicians. By contrast, there is very little research on paragrammatism,
and clinical practitioners are often unaware of its existence at all, leaving potential grammat-
ical deficits in aphasia undiagnosed. Agrammatism is associated with nonfluent aphasia, pri-
marily Broca’s aphasia (Damasio, 1992; Goodglass, 1993; Saffran, Berndt, & Schwartz, 1989;
Thompson, Lange, Schneider, & Shapiro, 1997), while paragrammatism is associated with flu-
ent aphasia, such as Wernicke’s and conduction aphasia (Goodglass, Christiansen, &
Gallagher, 1993). While recent lesion-behavior mapping studies have associated agrammatic
speech with damage to primarily frontal structures, particularly Broca’s area (den Ouden et al.,
2019; Sapolsky et al., 2010; Wilson et al., 2010), only a few case studies suggest an associ-
ation of paragrammatism with posterior temporal-parietal damage (Wilson, Eriksson, Schneck,
& Lucanie, 2018; Wilson, Yen, & Eriksson, 2018; Yagata et al., 2017). Consistent with this,
fluent aphasia is mostly associated with posterior temporal-parietal lesions (Buchsbaum
et al., 2011; Ogar et al., 2011; Yourganov, Smith, Fridriksson, & Rorden, 2015). However,
there have yet to be any large-scale lesion-symptom–mapping studies of paragrammatic def-
icits per se. Therefore, in the present work, we sought to identify the lesion distribution asso-
ciated with paragrammatism as distinct from agrammatism using voxel-based lesion-symptom
mapping in a large cohort of people with chronic aphasia following left-hemisphere stroke.
An important issue concerning research into syntactic deficits in aphasia is the question of
how syntax is organized in the healthy brain. While prominent models of syntax in the brain
posit a primary syntactic function to different subregions of the inferior frontal gyrus (IFG;
Friederici, 2017; Hagoort, 2014), Matchin and Hickok (2019) recently hypothesized a new
model of syntax in the brain, with two primary cortical zones responsible for distinct aspects
of syntactic processing. The first is a hierarchical lexical-syntactic system in the left posterior
middle temporal gyrus (pMTG), including the ventral bank of the superior temporal sulcus.
This system underlies hierarchical structures necessary for conceptual-semantic processing
that are critical for both comprehension and production of language (Everaert, Huybregts,
Chomsky, Berwick, & Bolhuis, 2015). The second is a linear morphosyntactic system in the
left inferior frontal gyrus, pars triangularis (IFGtri). This system underlies linear morphosyntac-
tic relations (such as word order and affixation rules) that are critical for producing speech
through the vocal tract, which is primarily a serial system (Berwick & Chomsky, 2016;
Idsardi & Raimy, 2013). However, the IFGtri is not strictly necessary for comprehension, as
comprehension does not require the explicit computation of serial relations, which are provided
by the incoming sequence of morphological inputs (Lewis & Vasishth, 2005).
Thus, Matchin and Hickok (2019) predict that damage to pMTG impairs both syntactic com-
prehension and production, whereas damage to IFGtri primarily impairs syntactic production
Neurobiology of Language
209
l
D
o
w
n
o
a
d
e
d
f
r
o
m
h
t
t
p
:
/
/
d
i
r
e
c
t
.
m
i
t
.
e
d
u
n
o
/
l
/
l
a
r
t
i
c
e
-
p
d
f
/
/
/
/
1
2
2
0
8
1
8
6
7
6
9
6
n
o
_
a
_
0
0
0
1
0
p
d
/
.
l
f
b
y
g
u
e
s
t
t
o
n
0
7
S
e
p
e
m
b
e
r
2
0
2
3
Agrammatism and paragrammatism
(with potential deficits for comprehension of complex sentences due to confounding effects of
impaired working memory resources; Matchin, 2018; Rogalsky & Hickok, 2011). However,
the model also predicts asymmetric production deficits following from damage to these two
systems: paragrammatic production deficits result from damage to the hierarchical lexical-
syntactic system in the pMTG, whereas agrammatic production deficits result from damage
to the linear morphosyntactic system in the IFGtri. This is the prediction we tested in the cur-
rent study.
We identified patients’ grammatical deficits through a perceptual rating of patients’
speech samples. According to the hypothesis presented in Matchin and Hickok (2019),
we expected a double dissociation: paragrammatism would be associated with damage to
the pMTG (and not IFGtri) while agrammatism would be associated with damage to IFGtri
(and not the pMTG). Because neuroimaging studies have also identified syntactic effects in
neighboring tissue (see Matchin & Hickok, 2019, for a review), and the difficulty of straight-
forwardly interpreting the localization in lesion-symptom mapping (Wilson, 2017), we cre-
ated broader regions of interest (ROIs) encompassing these regions to maximize our ability to
detect effects.
Importantly, the agrammatism/paragrammatism distinction has been argued to be governed
by fluency rather than by a fundamental underlying grammatical distinction. From this per-
spective, both patient groups may have the same grammatical deficit, but agrammatic patients’
speech production problems prevent them from producing much output at all, whereas para-
grammatic patients’ intact speech production allows them to produce voluminous disordered
output (Heeschen, 1985; Heeschen & Kolk, 1988; Kolk & Heeschen, 1992). Therefore, in sec-
ondary analyses we included a speech rate measure (words per minute) as a covariate to ac-
count for potential confounding effects of overall speech fluency.
A note on notation: throughout this article, we express the general concepts discussed in
the literature of agrammatism (and agrammatic speech) and paragrammatism (and paragram-
matic speech) using regular typeface. We express the corresponding perceptual classification
of these concepts as applied to our subject groups using small capital typeface, that is,
AGRAMMATISM/AGRAMMATIC and PARAGRAMMATISM/PARAGRAMMATIC.
PROCEDURE
Subjects
We initially analyzed connected speech samples from 100 people (28 women) with chronic
poststroke aphasia, which were collected as part of larger studies at the University of South
Carolina and the Medical University of South Carolina. All subjects were recruited through
local advertisement. They provided informed consent to participate in this study, which was
approved by the Institutional Review Boards at the University of South Carolina and the
Medical University of South Carolina. All subjects had a single ischemic stroke to the left
hemisphere at least six months prior to study inclusion and were also premorbidly right-
handed (self-disclosed). On average, subjects were 59.2 years old at time of testing
(±11.15 years), were 47.22 months poststroke (± 47.78 months), had 14.89 years of edu-
cation (± 2.41 years) and a Western Aphasia Battery-Revised (WAB-R) aphasia quotient of
58.70 (± 21.30; Kertesz, 2007). Out of the initial 100 subjects, the proportions of the
following aphasia types were included: 19 with anomia, 50 with Broca’s aphasia, 17 with con-
duction aphasia, six with global aphasia, two with transcortical motor aphasia, and six with
Wernicke’s aphasia.
Western Aphasia Battery (WAB):
battery of tests to assess language
abilities. Performance is used to
identify and classify aphasia in people
with neurological dysfunction.
Neurobiology of Language
210
l
D
o
w
n
o
a
d
e
d
f
r
o
m
h
t
t
p
:
/
/
d
i
r
e
c
t
.
m
i
t
.
e
d
u
n
o
/
l
/
l
a
r
t
i
c
e
-
p
d
f
/
/
/
/
1
2
2
0
8
1
8
6
7
6
9
6
n
o
_
a
_
0
0
0
1
0
p
d
.
/
l
f
b
y
g
u
e
s
t
t
o
n
0
7
S
e
p
e
m
b
e
r
2
0
2
3
Agrammatism and paragrammatism
Classification of Grammatical Deficits
Clinical rating scales have been developed for agrammatism, such as the Boston Diagnostic
Aphasia Examination grammatical form measure (Goodglass, Kaplan, & Barresi, 2000).
However, no modern evaluative tools exist for classification of paragrammatism. We therefore
relied on qualitative consensus assessments of expert raters, using the traditional Kleist (1914)
criteria for agrammatism and paragrammatism. To elicit speech, we followed the story retelling
protocol from AphasiaBank (MacWhinney, Fromm, Forbes, & Holland, 2011). Subjects first re-
viewed a picture book of the Cinderella story (text omitted), then the book was removed and they
were asked to retell the Cinderella story in their own words. Video recordings were made, lasting
from a few seconds to more than five minutes. Subjects were instructed to use content from the
book and their own recollection. Four expert raters (authors WM, AB, BS, DdO), blind to the
subject’s aphasia type, psychological assessment scores, and lesions, individually watched these
recordings and rated each subject as AGRAMMATIC, PARAGRAMMATIC, NO GRAMMATICAL DEFICIT (NGD, i.e.,
no specific grammatical deficit, with possible presence of other aphasic deficits) or CANNOT RATE
based on informal perceptual judgments. Raters were allowed to listen to each video as many
times as they liked. Following individual rating of each of the 100 subjects, a discussion was held
with all four experts to resolve disagreements about each case and to determine a consensus rat-
ing. Patients exhibiting features of both agrammatism and paragrammatism were classified as
BOTH (AGRAMMATIC and PARAGRAMMATIC). All raters were experienced language scientists, with a
mix of backgrounds in stroke and aphasia research, speech-language pathology, and linguistics.
PARAGRAMMATIC errors were classified as those not resulting from an overall reduction or omis-
sion of function words/morphemes or structures, but rather grammatical errors with a general
presence of functional elements. Using these criteria, individual PARAGRAMMATIC errors could be
omissions. For instance, the utterance “…and they’re visit” is ungrammatical because of the
omission of the progressive morpheme “-ing.” However, this subject did not appear to omit
inflections generally (indeed, the progressive auxiliary “are” is present in the verb contraction
in the same utterance), therefore such utterances were taken as evidence for PARAGRAMMATISM
rather than AGRAMMATISM. AGRAMMATIC subjects by contrast were defined as having an overall def-
icit of functional word and morpheme omission and reduced sentence complexity.
Of the 100 original subjects, we successfully rated 53, and these were included in the fol-
lowing analyses. Forty-seven subjects were unable to be rated due to audio quality issues (N =
2) or severely limited speech output or reduced intelligibility as a result of concomitant motor
speech problems (apraxia of speech and/or dysarthria) or severe aphasia (N = 45). Of the 53
successfully classified subjects, 21 were assigned to the PARAGRAMMATIC group, 11 to the
AGRAMMATIC group, and 17 to the NGD group. Four subjects were classified as BOTH
(AGRAMMATIC and PARAGRAMMATIC) based on the presence of both features in these subjects’
speech. Table 1 provides demographic data for each classified group. While Broca’s aphasia
was closely associated with AGRAMMATISM, and Wernicke’s and conduction aphasia were closely
associated with PARAGRAMMATISM, a variety of aphasia subtypes were classified within each gram-
matical category. As lesion volume was significantly larger in the AGRAMMATIC group, all of our
lesion-symptom mapping analyses included lesion volume as a covariate.
Examples of AGRAMMATIC errors (in subjects classified as AGRAMMATIC only)
Subject 127: “Cinderella very dress up”
Subject 127: “Cinderella one shoe”
Subject 129: “two girls and boy bad”
Neurobiology of Language
211
l
D
o
w
n
o
a
d
e
d
f
r
o
m
h
t
t
p
:
/
/
d
i
r
e
c
t
.
m
i
t
.
e
d
u
n
o
/
l
/
l
a
r
t
i
c
e
-
p
d
f
/
/
/
/
1
2
2
0
8
1
8
6
7
6
9
6
n
o
_
a
_
0
0
0
1
0
p
d
/
.
l
f
b
y
g
u
e
s
t
t
o
n
0
7
S
e
p
e
m
b
e
r
2
0
2
3
Aphasia
diagnosis
3 anomia,
6 Broca’s,
13 conduction,
3 Wernicke’s
1 anomia,
12 Broca’s,
1 conduction,
1 global
10 anomia,
6 Broca’s,
1 conduction
Agrammatism and paragrammatism
Table 1. Demographic information for each group of subjects
PARAGRAMMATIC
Number
25
Sex
9 Female
Age
(years)
62.16*
(9.91)
Months
poststroke
43.52*
(36.42)
Education
(years)
15.04^
(2.25)
Number w/
AOS
8*
WAB
AQ
63.50^
(17.51)
Lesion
volume
(cm3)
108.78*
(74.53)
AGRAMMATIC
15
6 Female
51.40*^
(13.60)
79.07*
(56.09)
16.07
(2.89)
12*^
61.41^
(12.92)
212.66*^
(55.11)
l
D
o
w
n
o
a
d
e
d
f
r
o
m
h
t
t
p
:
/
/
d
i
r
e
c
t
.
m
i
t
.
e
d
u
n
o
/
l
/
l
a
r
t
i
c
e
-
p
d
f
/
/
/
/
1
2
2
0
8
1
8
6
7
6
9
6
n
o
_
a
_
0
0
0
1
0
p
d
/
.
l
f
b
y
g
u
e
s
t
t
o
n
0
7
S
e
p
e
m
b
e
r
2
0
2
3
NGD
BOTH
17
4 Female
61.06
(12.71)
66.71
(76.51)
4
2 Female
50.75
(15.90)
91.00
(47.94)
16.41
(2.00)
16.50
(3.42)
7
2
80.28
(14.02)
80.66
(73.81)
65.18
(12.51)
150.64
(38.92)
3 Broca’s,
1 conduction
Note. NGD = NO GRAMMATICAL DEFICIT; AOS = apraxia of speech; WAB AQ = performance on the Western Aphasia Battery summary measure for overall aphasia
severity. Four subjects classified as BOTH (i.e., showing features of both AGRAMMATISM and PARAGRAMMATISM) were included in the AGRAMMATIC and PARAGRAMMATIC
groups shown here, as well as separately.
* Significant difference ( p < 0.05) between the PARAGRAMMATIC and AGRAMMATIC groups.
^Significant difference between PARAGRAMMATIC/AGRAMMATIC and NO GRAMMATICAL DEFICIT.
Subject 183: “daughters angry and uh sad”
Subject 183: “Cinder[ella]…poor…and no rooms”
Subject 1040: “fairy…um…Cinderella dress pretty…far away kinda…uh…the wish upon a
star…um…the horse pretty and…”
Subject 1040: “Cinderella all dressed and…slippers”
Subject 171: “a man…slippers…and…look…”
Subject 171: “and slipper…fit”
Subject 171: “and…crown…and…married”
Examples of PARAGRAMMATIC errors (in subjects classified as PARAGRAMMATIC only)
Subject 1034: “to live his father and stepmother” – verb complement selection violation
Subject 1034: “three other sister” – number agreement error
Subject 1034: “he had to do all the works” – incorrect plural inflection of mass noun
Subject 1034: “wanted to make a trick her” – fusion error: trick is both a noun and a verb
Subject 1041: “she came the house” – verb complement selection violation
Neurobiology of Language
212
Agrammatism and paragrammatism
Subject 1007: “she goed back to the boy” – use of regular past tense inflection for irregular
verb
Subject 1010: “tooked her dress” – use of regular past tense inflection in addition to irreg-
ular past tense formation
Subject 170: “one stepfather and a stepchildren” – number agreement error
Subject 184: “and she got the flied” – verb in noun position; regular past tense inflection on
irregular verb
Subject 194: “all they want to do is look the pretty” – article inserted incorrectly
Subject 194: “one of her slippers that were glass” – number agreement error
Subject 194: “I want to find this girl that I saw you” – pronoun inserted into gap of relative
clause
Subject 194: “she ran the steps” – verb complement selection violation
Subject 198: “she was met the prince” – incorrect auxiliary
Subject 198: “she turned out to the same person” – dropping of copula from infinitive
Subject 198: “the some happen to them” – multiple articles without noun
Subject 201: “this is not what good” – unclear construction, perhaps omission of auxiliary
(“what was good” -> “what good”)
Subject 201: “had something was going to back” – strange construction; omission of article
inside prepositional phrase (to the back -> to back)
l
D
o
w
n
o
a
d
e
d
f
r
o
m
h
t
t
p
:
/
/
d
i
r
e
c
t
.
m
i
t
.
e
d
u
n
o
/
l
/
l
a
r
t
i
c
e
–
p
d
f
/
/
/
/
1
2
2
0
8
1
8
6
7
6
9
6
n
o
_
a
_
0
0
0
1
0
p
d
/
.
l
Subject 209: “two women is ugly” – number agreement error
Subject 209: “two ugly child was” – number agreement error(s)
Subject 209: “two man” – number agreement error
Subject 209: “the queen and king is there” – number agreement error
Subject 209: “the Cinderella is found in the one” – incorrect use of definite article for proper
name
f
b
y
g
u
e
s
t
t
o
n
0
7
S
e
p
e
m
b
e
r
2
0
2
3
Subject 143: “she flied around” – use of regular past tense inflection for irregular verb
Subject 143: “and they’re visit” – omission of progressive inflection
Examples errors in subjects classified as BOTH (both AGRAMMATIC and PARAGRAMMATIC)
Subject 1002: “the girl run” – omission of verb inflection
Subject 1002: “And…evil woman…and locked the door” – telegraphic
Subject 1002: “The twins and evil mother” – omission of article on second noun of conjunct
Subject 1002: “It is girls” – agreement error
Subject 1002: “The girl is what can we do” – sentence monster
Neurobiology of Language
213
Agrammatism and paragrammatism
Subject 1002: “And the prince and the Cinderella is happily forever” – agreement error,
incorrect use of definite article for proper name
Subject 1024: “Cinderella cleaning so nice” – telegraphic
Subject 1024: “Cinderella is not going because I think that list” – telegraphic
Subject 1024: “so…different dress and…” – telegraphic
Subject 1024: “but mom is list for cleaning, vacuum, whatever” – telegraphic, perhaps
sentence monster
Subject 1024: “Cinderella you need to go [be]fore midnight because it’s broke your, spell
your broken” – sentence monster
Subject 1024: “Cinderella and prince is going to marry” – number agreement error
Subject 1044: “Cinderella is good” – simplification of sentence structure
Subject 1044: “slippers in the drawer is no good” – omission of definite determiner, agreement
error
Subject 1044: “Cinderella is danced with her maid” – incorrect inflection (substitution of
-ed for -ing)
Subject 190: “There’s girl and boy” – simplification of sentence structure, omission of
articles
Subject 190: “The other one, bad…bad…” – omission of copula
Subject 190: “The other one, bad bad” – omission of copula
Subject 190: “Everything nice” – omission of copula
Subject 190: “The girl…he’s really nice” – gender agreement error
Subject 190: “It’s moving the talking” – sentence monster
l
D
o
w
n
o
a
d
e
d
f
r
o
m
h
t
t
p
:
/
/
d
i
r
e
c
t
.
m
i
t
.
e
d
u
n
o
/
l
/
l
a
r
t
i
c
e
–
p
d
f
/
/
/
/
1
2
2
0
8
1
8
6
7
6
9
6
n
o
_
a
_
0
0
0
1
0
p
d
.
/
l
Reliability
To determine interrater agreement, each of the four expert raters individually rerated videos
from n = 10 subjects, that is, >20% of the sample that could be rated. Fleiss’s kappa was used
to determine rater agreement between each of the four raters. There was “good” agreement
between each rater, k = 0.61, (95% CI, 0.44 to 0.77), p < 0.0001. Individual kappa for each of
grammatical classification ranged from “fair” (PARAGRAMMATIC classification, k = 0.25) to “good”
(BOTH, NGD, k = 0.67 for both classifications) and “very good” (AGRAMMATIC classification, k =
0.90). Consensus agreement was also computed demonstrating the extent to which the first
consensus discussion helped with rater clarity and reliability for subject classification.
Cohen’s kappa was used to confirm reliability of rater criteria following the consensus agree-
ment meetings. Cohen’s kappa was 0.86, p < 0.0001, suggesting strong reliability for consen-
sus rating criteria.
f
b
y
g
u
e
s
t
t
o
n
0
7
S
e
p
e
m
b
e
r
2
0
2
3
Speech Fluency and Speech Rate
To avoid a similar conflation of grammatical abilities with ability from overall speech fluency,
we incorporated a speech rate dimension, words per minute ( WPM), as a covariate in second-
ary analyses. WPM was calculated based on CHAT/CLAN (talkbank.org/) transcriptions of
each subject’s speech during the same Cinderella task that was used for assessment of
Neurobiology of Language
214
Agrammatism and paragrammatism
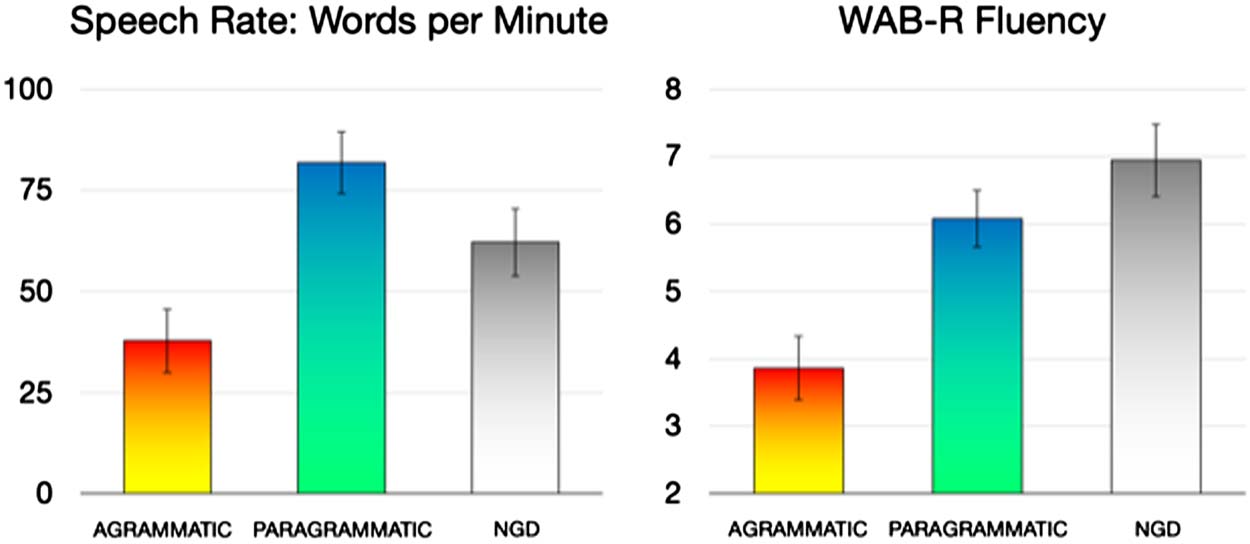
Figure 1.
Speech fluency, as measured in words per minute during the Cinderella story (left), and
the Western Aphasia Battery-Revised (WAB-R) fluency measure (right). NGD = NO GRAMMATICAL DEFICIT.
Error bars reflect standard error of the mean.
grammatical deficits (MacWhinney, 2000). Speech was transcribed by a speech pathology
masters student, using audiovisual speech recordings. Speech rate, as measured in WPM,
is shown in Figure 1 (left). For comparison, scores from the WAB-R fluency rating scale
(Kertesz, 2007) are shown in Figure 1 (right). For both measures, the AGRAMMATIC group (including
the subjects categorized as “both”) were the least fluent. With respect to the PARAGRAMMATIC
and NGD groups, the two measures diverged. For WPM, the PARAGRAMMATIC group was most
fluent, while for WAB-R fluency, the NGD group was most fluent. This is because the WAB-R
fluency scale incorporates both quantity and quality (e.g., grammatical deficits) of speech
output, whereas WPM measures speech rate regardless of quality.
Neuroimaging Data Acquisition and Processing
We acquired anatomical MRIs and performed lesion mapping using the same parameters and
procedures as described in Fridriksson et al. (2018). Neuroimaging data were collected at the
University of South Carolina (USC; 15 subjects) and the Medical University of South Carolina
(MUSC; 38 subjects). Lesions were demarcated onto each subject’s T2 image by an expert
technician (Roger Newman-Norlund, data from USC) or an expert neurologist (Leo Bonilha,
data from MUSC) blind to the behavioral data. Lesion overlap maps for each group included in
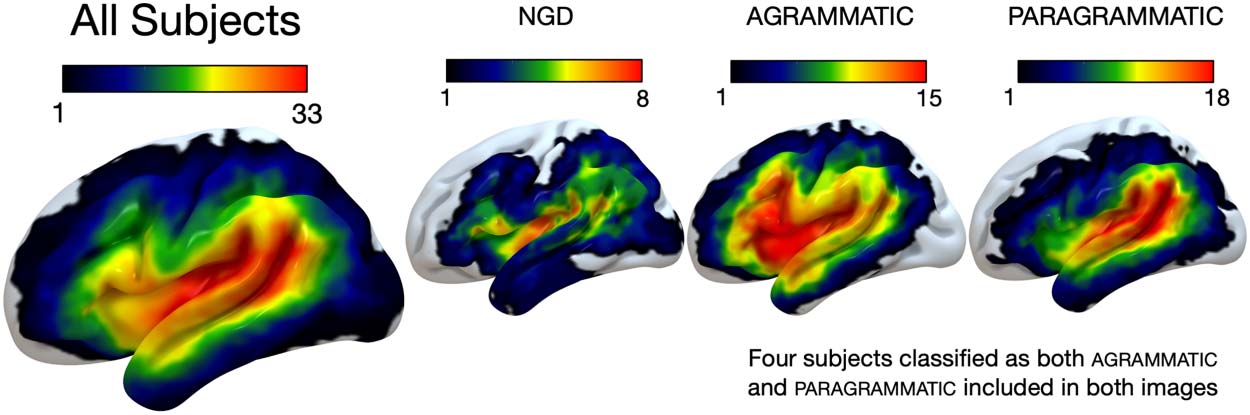
final analyses are shown in Figure 2.
Lesion overlap maps for each group. All Subjects (N = 53, max overlap = 33), NO
Figure 2.
GRAMMATICAL DEFICIT (NGD; N = 17, max overlap = 8), AGRAMMATIC (N = 15, max overlap = 15),
PARAGRAMMATIC (N = 25, max overlap = 18).
Neurobiology of Language
215
l
D
o
w
n
o
a
d
e
d
f
r
o
m
h
t
t
p
:
/
/
d
i
r
e
c
t
.
m
i
t
.
e
d
u
n
o
/
l
/
l
a
r
t
i
c
e
-
p
d
f
/
/
/
/
1
2
2
0
8
1
8
6
7
6
9
6
n
o
_
a
_
0
0
0
1
0
p
d
.
/
l
f
b
y
g
u
e
s
t
t
o
n
0
7
S
e
p
e
m
b
e
r
2
0
2
3
Agrammatism and paragrammatism
ROI Analyses
We created two ROIs by combining preexisting parcellations from the Johns Hopkins
University atlas (Faria et al., 2012). The Broca’s area ROI was created by combining the left
IFGtri, and pars opercularis. The left posterior superior and middle temporal gyri (pSTG/MTG)
ROI was created by combining the posterior superior temporal gyrus and middle temporal
gyrus. For each subject, we calculated percent damage to each ROI, and then calculated
residual percent damage values after performing a linear regression in SPSS (ibm.com/an) with
(i) lesion volume only as a covariate, and (ii) lesion volume and speech rate ( WPM) as covariates.
We then entered these residual values into independent samples t tests in SPSS, evaluating the
effect of AGRAMMATISM (subjects classified as AGRAMMATIC vs. subjects not classified as AGRAMMATIC)
and PARAGRAMMATISM (subjects classified as PARAGRAMMATIC vs. subjects not classified as
PARAGRAMMATIC) within each ROI.
To ensure that lesion volume was not distributed differently between the AGRAMMATIC and
PARAGRAMMATIC groups within these ROIs, we calculated Levine’s statistic testing for homoge-
neity of variances between these groups (based on median percent damage, Brown-Forsythe
test). The homogeneity of variance was not shown to be different between the AGRAMMATIC and
PARAGRAMMATIC groups within either the Broca’s area ROI, W(1,38) = 1.567, p = 0.218, or the
pSTG/MTG ROI, W (1,38) = 0.027, p = 0.869. Thus, our use of the lesion volume covariate did
not appear to interact differently with the distinction between AGRAMMATISM and PARAGRAMMATISM
within these ROIs. We also show ROI data without lesion volume covariates in the Supporting
Information (Figure S1).
l
D
o
w
n
o
a
d
e
d
f
r
o
m
h
t
t
p
:
/
/
d
i
r
e
c
t
.
m
i
t
.
e
d
u
n
o
/
l
/
l
a
r
t
i
c
e
-
p
d
f
/
/
/
/
1
2
2
0
8
1
8
6
7
6
9
6
n
o
_
a
_
0
0
0
1
0
p
d
.
/
l
f
b
y
g
u
e
s
t
t
o
n
0
7
S
e
p
e
m
b
e
r
2
0
2
3
Whole-Brain Analyses
We performed corresponding whole-brain analyses in NiiStat (https://www.nitrc.org/projects/
niistat/), using binary logistic regression to remove effects of (i) lesion volume only and (ii) le-
sion volume and speech rate ( WPM) from the behavioral classifications. We then performed
one-tailed t tests, using an uncorrected individual voxel-wise threshold of p < 0.05. Only vox-
els that were damaged in at least 5 subjects (~10% of sample) were included in the analyses.
We also show uncorrected whole-brain results using a stricter statistical threshold, p < 0.001,
in the Supporting Information (Figure S3).
To ensure that lesion volume across the whole brain was not distributed differently between
the AGRAMMATIC and PARAGRAMMATIC groups, we calculated Levine’s statistic testing for homoge-
neity of variances between these groups (based on median percent damage, Brown-Forsythe
test). The homogeneity of variance of whole-brain lesion volume was not shown to be different
between the AGRAMMATIC and PARAGRAMMATIC groups, W(1,38) = 1.851, p = 0.182. Thus, our use
of the lesion volume covariate did not appear to interact differently with the distinction be-
tween AGRAMMATISM and PARAGRAMMATISM at the whole-brain level. We also show whole-brain
results without lesion volume covariates in the Supporting Information (Figure S2).
RESULTS
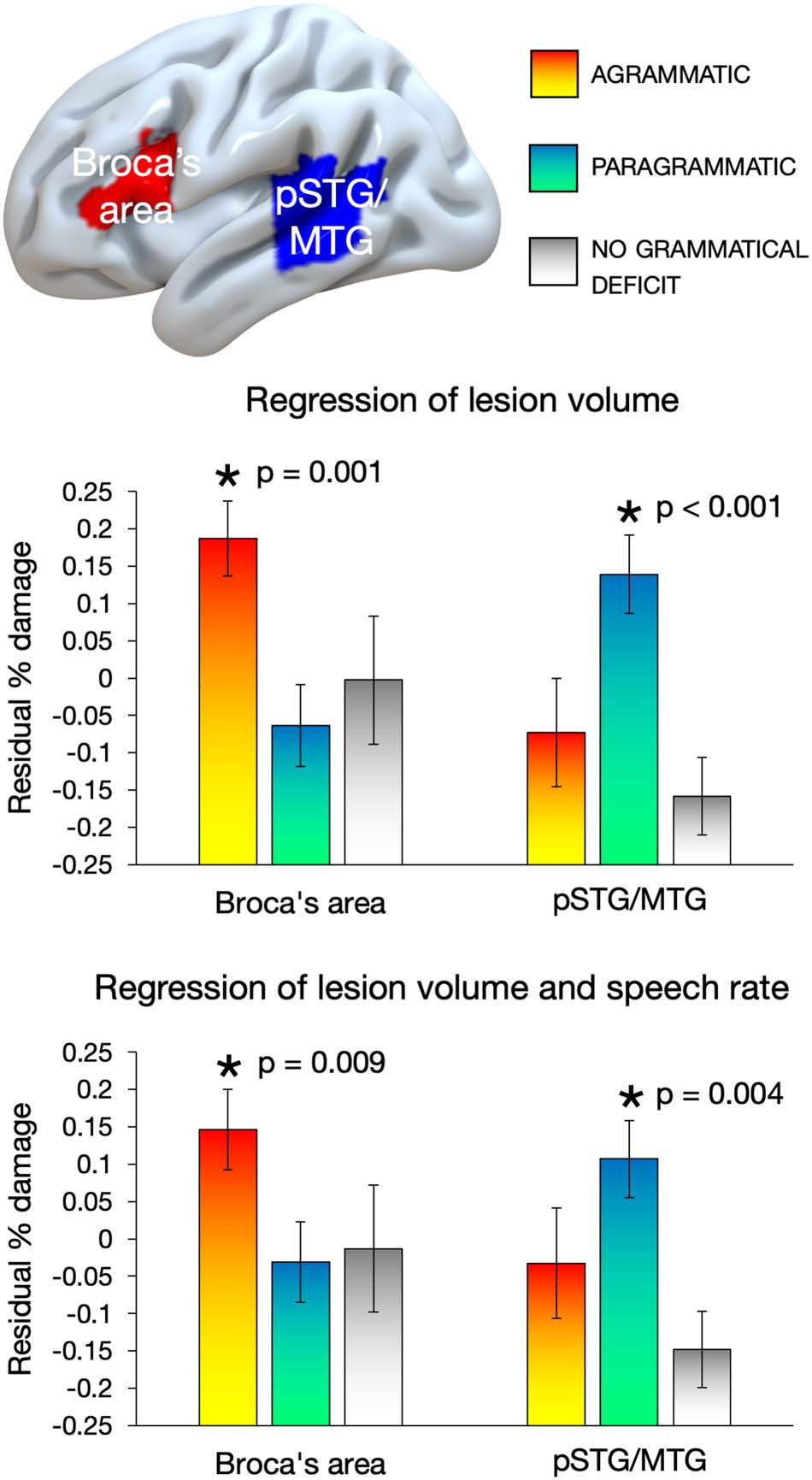
Figure 3 shows results from the ROI analyses. The results revealed a clear double dissociation:
when including only lesion volume as a covariate, AGRAMMATISM was significantly associated
with damage to Broca’s area, t(51) = 3.133, p = 0.001, but not pSTG/MTG, t(51) = −1.152, p =
0.873, while PARAGRAMMATISM was significantly associated with damage to pSTG/MTG, t(51) =
3.674, p < 0.001, but not Broca’s area, t(51) = −1.499, p = 0.930. These results also held when
Neurobiology of Language
216
Agrammatism and paragrammatism
l
D
o
w
n
o
a
d
e
d
f
r
o
m
h
t
t
p
:
/
/
d
i
r
e
c
t
.
m
i
t
.
e
d
u
n
o
/
l
/
l
a
r
t
i
c
e
-
p
d
f
/
/
/
/
1
2
2
0
8
1
8
6
7
6
9
6
n
o
_
a
_
0
0
0
1
0
p
d
.
/
l
f
b
y
g
u
e
s
t
t
o
n
0
7
S
e
p
e
m
b
e
r
2
0
2
3
Figure 3. Double dissociation between the effect of AGRAMMATISM and the effect of PARAGRAMMATISM
with respect to damage in Broca’s area and the posterior superior and middle temporal gyri (pSTG/
MTG) regions of Interest (ROIs). Top: selected ROIs. Residual values of average percent damage for
each group to each ROI, after regressing out lesion volume (LV; middle) and after regressing out
both LV and words per minute (bottom) using linear regression in SPSS. Error bars reflect standard
error of the mean. Asterisks indicate significant effects when performing a Bonferroni correction for
multiple comparisons and an alpha of 0.0125. Four subjects classified as BOTH (both AGRAMMATIC and
PARAGRAMMATIC) were included in both analyses.
adding speech rate as a covariate: AGRAMMATISM was significantly associated with damage to
Broca’s area, t(51) = 2.458, p = 0.009, but not pSTG/MTG, t(51) = −0.528, p = 0.700, while
PARAGRAMMATISM was significantly associated with damage to pSTG/MTG, t(51) = 2.786, p =
0.004, but not Broca’s area, t(51) = −0.744, p = 0.770.
In the Supporting Information, we show corresponding data without the lesion volume
covariate (Figure S1).
Neurobiology of Language
217
Agrammatism and paragrammatism
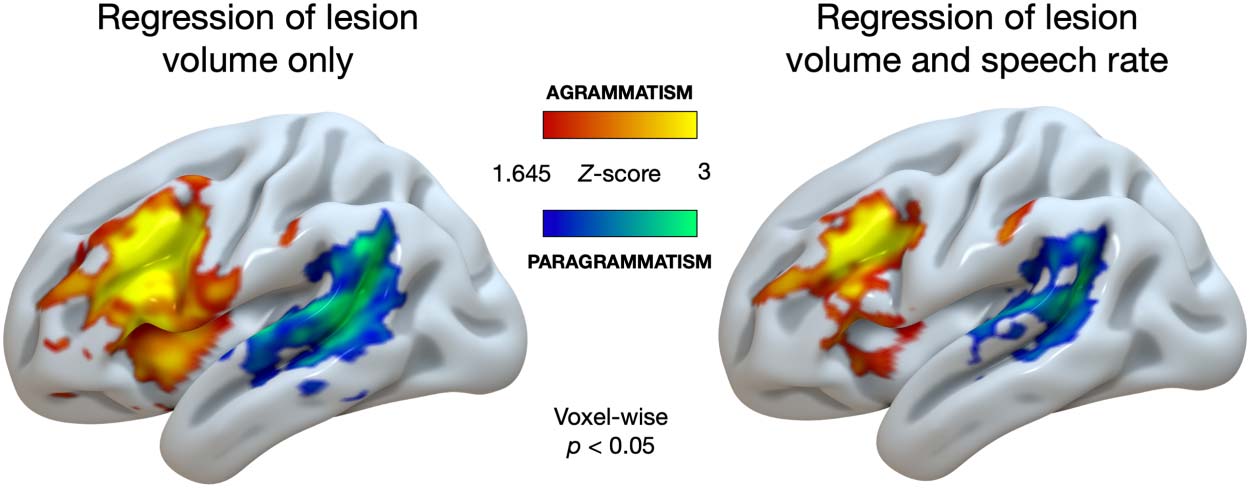
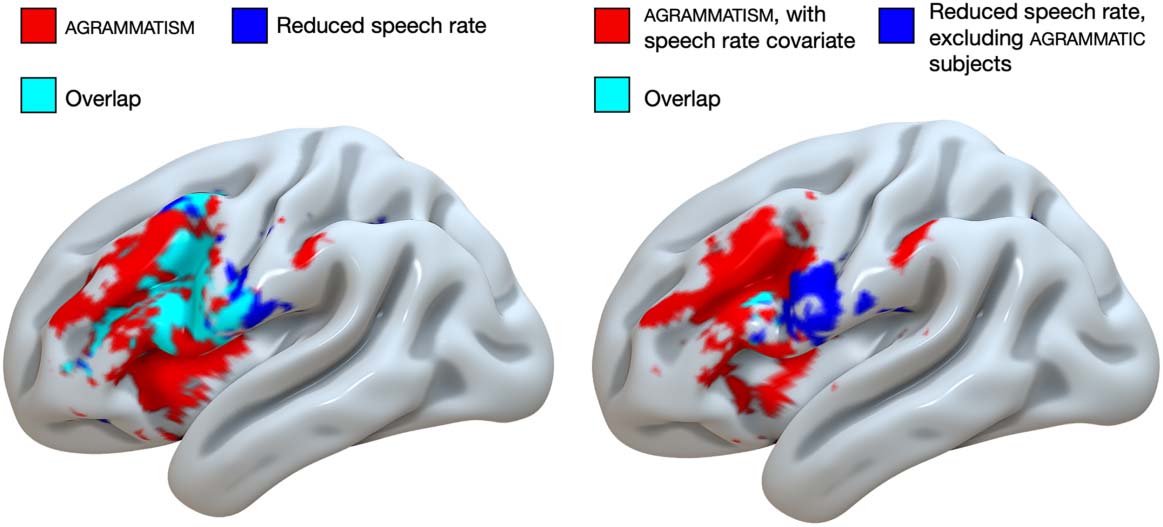
Figure 4. Uncorrected whole-brain analyses (voxel-wise p < 0.05) of the effects of AGRAMMATISM
(red-yellow) and PARAGRAMMATISM (blue-green) displayed on the cortical surface an inflated left-
hemisphere brain template in MNI space. Left: only lesion volume included as a covariate. Right:
both lesion volume and speech rate (words per minute) included as covariates. AGRAMMATISM = effect
of agrammatism (AGRAMMATIC, including BOTH > NO GRAMMATICAL DEFICIT and PARAGRAMMATIC, excluding
BOTH), PARAGRAMMATISM = effect of paragrammatism (PARAGRAMMATIC, including BOTH > NO GRAMMATICAL
DEFICIT and AGRAMMATIC, excluding BOTH).
Figure 4 shows the results of our whole-brain analyses (local maxima peak coordinates are
shown in Table 2). With respect to the effect of AGRAMMATISM (Figure 4, hot colors), both anal-
yses (with and without regression of WPM) revealed damage to the IFG and middle frontal
gyrus, encroaching into the insula, with minor damage to the anterior supramarginal gyrus
(SMG). When only including lesion volume as a covariate, AGRAMMATISM was also associated
with damage to left ventral precentral gyrus, but these effects were not present when speech
rate was included as a covariate. PARAGRAMMATISM (Figure 4, cool colors) was associated with
damage to left posterior temporal and inferior parietal cortex, centered on the posterior supe-
rior temporal gyrus and middle temporal gyrus, including the inferior and posterior parts of
the SMG. Overall, regressing out the effect of speech rate ( WPM) reduced the strength and
the spatial extent of the damage associated with AGRAMMATISM and PARAGRAMMATISM while
maintaining essentially the same spatial location. There was no spatial overlap in the damage
associated with each type of grammatical deficit, whether or not WPM was included as a
covariate.
In the Supporting Information, we show corresponding results without the lesion volume
covariate (Figure S2). We also show uncorrected whole-brain analyses at a stricter statistical
threshold ( p < 0.001; Figure S3).
To identify the relation between damage associated with agrammatism and impaired
speech rate, we performed uncorrected whole-brain analyses comparing the effects of reduced
WPM and AGRAMMATISM (Figure 5). Reduced WPM was associated with damage to left inferior
postcentral gyrus, precentral gyrus, middle frontal gyrus, and inferior frontal gyrus. There was
notable overlap between the lesion distribution associated with reduced WPM and
AGRAMMATISM in the left precentral gyrus and inferior frontal gyrus when only regressing lesion
volume. However, regressing out the effect of WPM from AGRAMMATISM, and removing
AGRAMMATIC subjects from the analysis of reduced WPM (i.e., only analyzing the effect of re-
duced WPM in patients without AGRAMMATISM, n = 38), revealed minimal overlap between
AGRAMMATISM and reduced WPM. Namely, reduced WPM in absence of AGRAMMATISM was asso-
ciated with damage to left inferior precentral gyrus, and AGRAMMATISM (covarying out WPM) was
associated with damage to left inferior and middle frontal gyrus.
Neurobiology of Language
218
l
D
o
w
n
o
a
d
e
d
f
r
o
m
h
t
t
p
:
/
/
d
i
r
e
c
t
.
m
i
t
.
e
d
u
n
o
/
l
/
l
a
r
t
i
c
e
-
p
d
f
/
/
/
/
1
2
2
0
8
1
8
6
7
6
9
6
n
o
_
a
_
0
0
0
1
0
p
d
/
.
l
f
b
y
g
u
e
s
t
t
o
n
0
7
S
e
p
e
m
b
e
r
2
0
2
3
Agrammatism and paragrammatism
Table 2. Local peak coordinates for the uncorrected whole-brain analyses (all coordinates in left hemisphere)
Region
PARAGRAMMATISM (regressing out the effect of lesion volume only)
Posterior superior temporal gyrus and sulcus
Temporal-parietal junction
Inferior parietal lobule/angular gyrus
Posterior middle temporal gyrus and superior temporal sulcus
Superior middle temporal gyrus
X
−47
−45
−46
−43
−51
PARAGRAMMATISM (regressing out the effect of lesion volume and words per minute)
Temporal-parietal junction
Superior temporal gyrus
Supramarginal gyrus
Middle temporal gyrus
Superior temporal gyrus
AGRAMMATISM (regressing out the effect of lesion volume only)
Postcentral gyrus
Inferior frontal gyrus (pars triangularis)
Inferior frontal gyrus (pars triangularis)/middle frontal gyrus
−42
−47
−55
−50
−57
−67
−53
−36
AGRAMMATISM (regressing out the effect of lesion volume and words per minute)
Inferior frontal gyrus (pars triangularis)
Inferior frontal gyrus (pars triangularis)/middle frontal gyrus
−53
−45
Y
−45
−50
−53
−39
−19
−51
−27
−48
−41
−37
−10
22
23
22
28
Z
11
19
32
2
5
20
8
31
−1
12
22
26
31
26
29
Z-value
3.97
4.05
4.38
4.15
3.86
3.59
3.00
3.20
3.14
3.41
3.98
5.22
4.85
4.74
4.50
Figure 5. Uncorrected whole-brain analyses (voxel-wise p < 0.05) of the effects of AGRAMMATISM (red),
reduced speech rate in words per minute (blue), and their overlap (cyan) displayed on the cortical surface
an inflated left-hemisphere brain template in MNI space. Left: only lesion volume included as a covariate.
Right: speech rate included as an additional covariate in the analysis of AGRAMMATISM (red), and excluding
AGRAMMATIC subjects in the analysis of reduced speech rate (blue, n = 38), with minimal overlap (cyan).
Neurobiology of Language
219
l
D
o
w
n
o
a
d
e
d
f
r
o
m
h
t
t
p
:
/
/
d
i
r
e
c
t
.
m
i
t
.
e
d
u
n
o
/
l
/
l
a
r
t
i
c
e
-
p
d
f
/
/
/
/
1
2
2
0
8
1
8
6
7
6
9
6
n
o
_
a
_
0
0
0
1
0
p
d
.
/
l
f
b
y
g
u
e
s
t
t
o
n
0
7
S
e
p
e
m
b
e
r
2
0
2
3
Agrammatism and paragrammatism
DISCUSSION
Our results revealed a clear double dissociation: AGRAMMATIC speech (but not PARAGRAMMATIC
speech) is significantly associated with damage to Broca’s area, while PARAGRAMMATIC speech
(but not AGRAMMATIC speech) is significantly associated with damage to pSTG/MTG. This double
dissociation held even when accounting for variability in speech rate (words per minute). The
association we identified between AGRAMMATISM and inferior and middle frontal damage is consis-
tent with previous lesion-deficit mapping studies (den Ouden et al., 2019; Sapolsky et al., 2010;
Wilson et al., 2010), and the association we observed between damage to left posterior temporal-
parietal cortex with PARAGRAMMATISM is consistent with previous case studies (Wilson, Eriksson,
et al., 2018; Wilson, Yen, & Eriksson, 2018; Yagata et al., 2017). The association of
PARAGRAMMATISM with posterior damage is also consistent with the general association of paragram-
matism with fluent aphasia, which typically involves damage to left posterior temporal-parietal
systems (Buchsbaum et al., 2011; Ogar et al., 2011), although we note that patients from both
fluent and nonfluent aphasias were present in both our AGRAMMATIC and PARAGRAMMATIC groups.
There has been strikingly little focus on understanding the nature of paragrammatism and its
neural correlates, in contrast to agrammatic speech, which has had a much greater focus
(Kean, 1985). This is in part due to the strong historical association of Broca’s aphasia and
agrammatism as reflecting a core syntactic deficit (Caramazza & Zurif, 1976; Grodzinsky,
1986, 2000; Schwartz, Saffran, & Marin, 1980), and a corresponding focus on the role of
the left IFG in syntax (Friederici, 2017; Grodzinsky & Santi, 2008). Our results drive home
the importance of considering paragrammatism as an independent grammatical disorder, re-
sulting from damage to distinct brain systems from those implicated in agrammatic speech.
The limited attention that has been paid to paragrammatism in past research has often been
in the service of the hypothesis that agrammatism and paragrammatism are different degrees of
adaptation to a common underlying deficit (Bates & Goodman, 1997; Bates & Wulfeck, 1989;
Heeschen, 1985; Heeschen & Kolk, 1988; Kolk & Heeschen, 1992), including a critique of the
supposed unique relation between Broca’s area damage and agrammatism (Dick et al., 2001).
This hypothesis is supported by the fact that paragrammatic errors can be observed in non-
fluent agrammatic speakers when they are forced to produce speech more quickly than their
natural pace (Heeschen & Kolk, 1988). However, the double dissociation we identified here,
which held even when incorporating words per minute as a covariate, speaks against this
hypothesis. Consistent with a more fundamental distinction between agrammatism and
paragrammatism, Casilio, Rising, Beeson, Bunton, and Wilson (2019) recently reported a
factor analysis for a large range of perceptual measures similarly extracted from connected
speech samples (N = 24 people with aphasia). They show that paragrammatism is sharply
distinguished from agrammatic features such as omission of function words/morphemes.
Paragrammatism was associated with a variety of speech deficits such as abandoned
utterances, empty speech, semantic paraphasias, phonemic paraphasias, and neologisms.
Nevertheless, we do note that many of the paragrammatic errors we identified here (particu-
larly inflectional errors such as agreement mismatch) do not follow straightforwardly from
lexical-semantic substitutions and appear to constitute a separate deficit.
An additional reason that previous research has focused largely on agrammatism to the
exclusion of paragrammatism is that it is difficult to clearly identify paragrammatism as dis-
tinct from these other disturbances to speech output. This is reflected in the relatively modest
interrater agreement of PARAGRAMMATISM that our expert raters obtained in this study (k = 0.25),
whereas the interrater agreement for AGRAMMATISM was much greater (k = 0.90). One potential
solution to this issue is to use an objective classification of paragrammatic deficits rather
Agreement:
dependency between two linguistic
elements (e.g., subject-verb agreement
in English, where -s on a verb indicates
a third person/singular subject).
Neurobiology of Language
220
l
D
o
w
n
o
a
d
e
d
f
r
o
m
h
t
t
p
:
/
/
d
i
r
e
c
t
.
m
i
t
.
e
d
u
n
o
/
l
/
l
a
r
t
i
c
e
-
p
d
f
/
/
/
/
1
2
2
0
8
1
8
6
7
6
9
6
n
o
_
a
_
0
0
0
1
0
p
d
.
/
l
f
b
y
g
u
e
s
t
t
o
n
0
7
S
e
p
e
m
b
e
r
2
0
2
3
Agrammatism and paragrammatism
than relying on a perceptual rating of paragrammatism (as in the present study and Casilio
et al., 2019). However, we were careful to note that isolated speech samples can be difficult
to characterize as agrammatic or paragrammatic using an objective criterion. This is because
if paragrammatism reflects a random misuse of grammar, omissions of functional elements
will occasionally result, incorrectly appearing to indicate agrammatism. Therefore, an impor-
tant contribution will be to develop clear diagnostic criteria for paragrammatism and to in-
vestigate the degree to which paragrammatic deficits can be separated from nongrammatical
deficits (such as lexical-semantic errors), including both subjective perceptual and objective
criteria.
The pSTG/MTG and Broca’s area have previously been implicated in syntactic process-
ing, with remarkably similar effects in both areas. They both exhibit increased activity for
grammatically structured linguistic materials relative to unstructured word lists regardless
of the richness of conceptual-semantic content (Goucha & Friederici, 2015; Matchin,
Hammerly, & Lau, 2017; Pallier, Devauchelle, & Dehaene, 2011), and damage to both re-
gions has been implicated in deficits comprehending syntactically complex materials (Tyler
et al., 2011). While these previous studies have shown largely similar syntactic effects in
both regions, the double dissociation revealed in the present study supports a functional dis-
tinction between them.
Previous lesion-deficit mapping studies of basic sentence and syntactic comprehension in
the absence of working memory confounds have also primarily identified similar left posterior
temporal-parietal areas (Fridriksson et al., 2018; den Ouden et al., 2019; Pillay, Binder,
Humphries, Gross, & Book, 2017; Rogalsky et al., 2018; Thothathiri, Kimberg, & Schwartz,
2012; Wilson & Saygın, 2004). This suggests a role for left posterior temporal-parietal cortex
in grammatical processes that underlie both comprehension and production. Matchin and
Hickok (2019) put forward the theory that left pMTG underlies hierarchical lexical-syntactic
structure, and that sentence comprehension and paragrammatic production deficits follow
from difficulties with hierarchical syntax. Consider paragrammatic errors such as incorrect
subject-verb number agreement, for example, “the queen and king is there.” Subject-verb
agreement in English must be calculated over structure. In the paragrammatic example,
both “queen” and “king” occur in the singular. However, the correct agreement feature is
plural: the verb agrees with the conjoined noun phrase, rather than the individual nouns.
Thus, the paragrammatic error can be seen as the lack of constraining hierarchical structural
relations.
Our results reinforce previous findings regarding the association of agrammatic production
and damage to the left inferior frontal cortex (den Ouden et al., 2019; Sapolsky et al., 2010;
Wilson et al., 2010). Broca’s area has long been associated with speech production, and most
current research supports a role for higher level planning of language rather than lower level
motor execution (Basilakos, Rorden, Bonilha, Moser, & Fridriksson, 2015; Flinker et al., 2015).
Matchin and Hickok (2019) suggest that the anterior portion of Broca’s area, the pars triangu-
laris, supports production via morphosyntactic sequences that are necessary for converting
hierarchical structures into linear speech output, and that when damaged, speech becomes
agrammatic.
On this point, we note that while previous research has found a general overlap between
effects of reduced speech rate and agrammatism (Wilson et al., 2010), the effect of AGRAMMATISM
we observed in left inferior and middle frontal cortex remained even when regressing out the
effect of speech rate (albeit somewhat weakened). Additionally, reduced speech rate in sub-
jects without AGRAMMATISM was associated with a distinct nonoverlapping cluster in inferior
Neurobiology of Language
221
l
D
o
w
n
o
a
d
e
d
f
r
o
m
h
t
t
p
:
/
/
d
i
r
e
c
t
.
m
i
t
.
e
d
u
n
o
/
l
/
l
a
r
t
i
c
e
-
p
d
f
/
/
/
/
1
2
2
0
8
1
8
6
7
6
9
6
n
o
_
a
_
0
0
0
1
0
p
d
/
.
l
f
b
y
g
u
e
s
t
t
o
n
0
7
S
e
p
e
m
b
e
r
2
0
2
3
Agrammatism and paragrammatism
precentral gyrus. Finally, a previous lesion-symptom mapping study distinguishing between
aphasia and apraxia of speech found that these syndromes strongly dissociate (Basilakos
et al., 2015). In that study, focusing on frontal cortex, apraxia of speech was associated with
damage to inferior precentral gyrus, whereas aphasia was associated with damage to anterior
inferior frontal gyrus (pars triangularis and pars orbitalis). In the present study, a large propor-
tion of the AGRAMMATIC speakers were indeed also diagnosed with apraxia of speech (12/15,
versus 8/25 of the PARAGRAMMATIC speakers). These previous results, however, including our re-
gression analysis, show that apraxia of speech cannot be the sole driving force behind agram-
matism and it is more likely that the two co-occur due to the anatomical proximity of their
neural substrates, even if these do not overlap.
Neither AGRAMMATISM nor PARAGRAMMATISM was associated with damage to the left anterior
temporal lobe (ATL) in our whole-brain analyses. The finding agrees with previous lesion-
symptom mapping studies of agrammatic production failing to identify effects in the ATL
(den Ouden et al., 2019; Sapolsky et al., 2010; Wilson et al., 2010). However, some previous
studies have reported associations between noncanonical sentence comprehension deficits
and damage to the left ATL in both chronic and acute stroke that might imply a syntactic func-
tion of this region (Dronkers, Wilkins, Van Valin, Redfern, & Jaeger, 2004; Magnusdottir et al.,
2013). We note that both of these studies did not control for lesion volume. As reported in the
Supporting Information (Figure S2), we show that AGRAMMATISM was in fact significantly associ-
ated with damage to the ATL when lesion volume was not included as a covariate. Given this,
we suggest that stroke-based lesion-symptom mapping studies of noncanonical sentence com-
prehension that control for lesion volume will identify effects primarily in left posterior tem-
poral areas and not the ATL, as reported by Rogalsky et al. (2018).
Although we started with a large sample (100 subjects), the difficulty in obtaining enough
speech output in the experimental task combined with the partitioning of subjects into distinct
groups resulted in less overall statistical power. Omitting subjects with low speech output also
likely precludes analysis of patients with both severe agrammatic and nonfluent speech. Thus,
patients who might be highly informative to our lesion-symptom mapping results are pre-
cluded by the nature of our approach: analyzing production during spontaneous discourse/
narration. These issues should be addressed in future studies.
Overall, the double dissociation identified here confirms the predictions of Matchin and
Hickok (2019): agrammatism (but not paragrammatism) follows from inferior frontal damage,
while paragrammatism (but not agrammatism) follows from posterior temporal damage. This
suggests that agrammatism and paragrammatism are distinct syndromes as opposed to reflect-
ing alternative adaptations to the same underlying grammatical deficit (Dick et al., 2001; Kolk
& Heeschen, 1992). Both basic research into the neural organization of language as well as
research into the nature of aphasia symptoms and recovery will benefit from increased focus
on paragrammatism itself and its distinction from agrammatism.
ACKNOWLEDGMENTS
We would like to thank Grigori Yourganov, Roger Newman-Norlund, Chris Rorden, and Leo
Bonilha for their technical assistance. We would also like to thank Leigh Ann Spell, Allison
Croxton, Anna Doyle, Michele Martin, Katie Murphy, and Sara Sayers for their assistance with
data collection, and graduate student clinicians in the Aphasia Lab for transcribing and coding
speech samples. Finally, we owe a debt of gratitude for Stephen Wilson and his laboratory,
who provided invaluable feedback on this work.
Neurobiology of Language
222
l
D
o
w
n
o
a
d
e
d
f
r
o
m
h
t
t
p
:
/
/
d
i
r
e
c
t
.
m
i
t
.
e
d
u
n
o
/
l
/
l
a
r
t
i
c
e
-
p
d
f
/
/
/
/
1
2
2
0
8
1
8
6
7
6
9
6
n
o
_
a
_
0
0
0
1
0
p
d
/
.
l
f
b
y
g
u
e
s
t
t
o
n
0
7
S
e
p
e
m
b
e
r
2
0
2
3
Agrammatism and paragrammatism
FUNDING INFORMATION
Julius Fridriksson, National Institute on Deafness and Other Communication Disorders (http://
dx.doi.org/10.13039/100000055), Award ID: P50 DC014664. Julius Fridriksson, National
Institute on Deafness and Other Communication Disorders (http://dx.doi.org/10.13039/
100000055), Award ID: U01 DC011739. Alexandra Basilakos, National Institute on
Deafness and Other Communication Disorders (http://dx.doi.org/10.13039/100000055),
Award ID: T32 DC 014435.
AUTHOR CONTRIBUTIONS
William Matchin: Conceptualization; Formal analysis – lead; Methodology; Resources – supporting;
Validation; Visualization – lead; Writing – original draft; Writing – review & editing – lead. Alexandra
Basilakos: Conceptualization – supporting; Formal analysis – supporting; Methodology; Resources –
lead; Validation; Writing – original draft – Supporting; Writing – review & editing – Supporting.
Brielle C. Stark: Conceptualization – supporting; Formal analysis – supporting; Methodology;
Validation; Writing – original draft – supporting; Writing – review & editing – supporting. Dirk den
Ouden: Conceptualization – supporting; Formal analysis – supporting; Methodology; Validation;
Writing – original draft – supporting; Writing – review & editing – supporting. Julius Fridriksson:
Conceptualization – supporting; Funding acquisition – lead; Methodology – supporting; Resources;
Writing – original draft – supporting; Writing – review & editing – Supporting. Gregory Hickok:
Conceptualization; Methodology – supporting; Writing – original draft – supporting; Writing –
review & editing – supporting.
REFERENCES
Basilakos, A., Rorden, C., Bonilha, L., Moser, D., & Fridriksson, J.
(2015). Patterns of poststroke brain damage that predict speech
production errors in apraxia of speech and aphasia dissociate.
S t r o k e , 4 6 ( 6 ) , 1 5 6 1 – 1 5 6 6 . h t t p s : / / d o i . o r g / 1 0 . 1 1 6 1 /
STROKEAHA.115.009211
Bates, E., & Goodman, J. C. (1997). On the inseparability of grammar
and the lexicon: Evidence from acquisition, aphasia and real-time
processing. Language and Cognitive Processes, 12(5–6), 507–584.
Bates, E., & Wulfeck, B. (1989). Comparative aphasiology: A cross-
linguistic approach to language breakdown. Aphasiology, 3(2),
111–142.
Berwick, R. C., & Chomsky, N. (2016). Why only us: Language and
evolution. Cambridge, MA: MIT Press.
Buchsbaum, B. R., Baldo, J., Okada, K., Berman, K. F., Dronkers,
N., D’Esposito, M., & Hickok, G. (2011). Conduction aphasia,
sensory-motor integration, and phonological short-term memory:
An aggregate analysis of lesion and fMRI data. Brain and
Language, 119(3), 119–128. https://doi.org/10.1016/j.
bandl.2010.12.001
Butterworth, B., & Howard, D. (1987). Paragrammatisms. Cognition,
26(1), 1–37. https://doi.org/10.1016/0010-0277(87)90012-6
Caramazza, A., & Zurif, E. B. (1976). Dissociation of algorithmic
and heuristic processes in language comprehension: Evidence
from aphasia. Brain and Language, 3(4), 572–582. https://doi.
org/10.1016/0093-934X(76)90048-1
Casilio, M., Rising, K., Beeson, P. M., Bunton, K., & Wilson, S. M.
(2019). Auditory-perceptual rating of connected speech in apha-
sia. American Journal of Speech-Language Pathology, 28(2),
550–568. https://doi.org/10.1044/2018_AJSLP-18-0192
Damasio, A. R. (1992) Aphasia. New England Journal of Medicine,
326, 531–539.
Den Ouden, D.-B., Malyutina, S., Basilakos, A., Bonilha, L.,
Gleichgerrcht, E., Yourganov, G., … Fridriksson, J. (2019).
Cortical and structuralconnectivity damage correlated with im-
paired syntactic processing in aphasia. Human Brain Mapping,
40(7), 2153–2173. https://doi.org/10.1002/hbm.24514
Dick, F., Bates, E., Wulfeck, B., Utman, J. A., Dronkers, N., &
Gernsbacher, M. A. (2001). Language deficits, localization, and
grammar: Evidence for a distributive model of language break-
down in aphasic patients and neurologically intact individuals.
Psychological Review, 108(4), 759–788. https://doi.org/
10.1037/0033-295X.108.4.759
Dronkers, N. F., Wilkins, D. P., Van Valin, R. D., Redfern, B. B., &
Jaeger, J. J. (2004). Lesion analysis of the brain areas involved in
language comprehension. Cognition, 92(1–2), 145–177. https://
doi.org/10.1016/j.cognition.2003.11.002
Everaert, M. B. H., Huybregts, M. A. C., Chomsky, N., Berwick, R. C., &
Bolhuis, J. J. (2015). Structures, not strings: Linguistics as part of the
cognitive sciences. Trends in Cognitive Sciences, 19(12), 729–743.
https://doi.org/10.1016/j.tics.2015.09.008
Faria, A. V., Joel, S. E., Zhang, Y., Oishi, K., van Zjil, P. C., Miller,
M. I., … & Mori, S. (2012). Atlas-based analysis of resting-state
functional connectivity: Evaluation for reproducibility and multi-
modal anatomy–function correlation studies. NeuroImage, 61(3),
613–621.
Flinker, A., Korzeniewska, A., Shestyuk, A. Y., Franaszczuk, P. J.,
Dronkers, N. F., Knight, R. T., & Crone, N. E. (2015).
Redefining the role of Broca’s area in speech. Proceedings of
Neurobiology of Language
223
l
D
o
w
n
o
a
d
e
d
f
r
o
m
h
t
t
p
:
/
/
d
i
r
e
c
t
.
m
i
t
.
e
d
u
n
o
/
l
/
l
a
r
t
i
c
e
-
p
d
f
/
/
/
/
1
2
2
0
8
1
8
6
7
6
9
6
n
o
_
a
_
0
0
0
1
0
p
d
.
/
l
f
b
y
g
u
e
s
t
t
o
n
0
7
S
e
p
e
m
b
e
r
2
0
2
3
Agrammatism and paragrammatism
the National Academy of Sciences, 112(9), 2871–2875. https://
doi.org/10.1073/pnas.1414491112
Fridriksson, J., den Ouden, D.-B., Hillis, A. E., Hickok, G., Rorden,
C., Basilakos, A., … Bonilha, L. (2018). Anatomy of aphasia re-
visited. Brain, 141(3), 848–862. https://doi.org/10.1093/ brain/
awx363
Friederici, A. D. (2017). Language in our brain: The origins of a
uniquely human capacity. Cambridge, MA: MIT Press.
Goodglass, H. (1993). Understanding aphasia. San Diego, CA:
Academic Press.
Goodglass, H., Christiansen, J. A., & Gallagher, R. (1993).
Comparison of morphology and syntax in free narrative and
structured tests: Fluent vs. nonfluent aphasics. Cortex, 29(3),
377–407.
Goodglass, H., Kaplan, E., & Barresi, B. (2000). Boston Diagnostic
Aphasia Examination (3rd ed.). Boston, MA: Pearson.
Goucha, T., & Friederici, A. D. (2015). The language skeleton after
dissecting meaning: A functional segregation within Broca’s
Area. NeuroImage, 114, 294–302. https://doi.org/10.1016/j.
neuroimage.2015.04.011
Grodzinsky, Y. (1986). Language deficits and the theory of syntax.
Brain and Language, 27(1), 135–159. https://doi.org/10.1016/
0093-934X(86)90009-X
Grodzinsky, Y. (2000). The neurology of syntax: Language use
without Broca’s area. Behavioral and Brain Sciences, 23(1), 1–21.
https://doi.org/10.1017/S0140525X00002399
Grodzinsky, Y., & Santi, A. (2008). The battle for Broca’s region.
Trends in Cognitive Sciences, 12(12), 474–480. https://doi.org/
10.1016/j.tics.2008.09.001
Hagoort, P. (2014). Nodes and networks in the neural architecture
for language: Broca’s region and beyond. Current Opinion in
Neurobiology, 28, 136–141. https://doi.org/10.1016/j.
conb.2014.07.013
Heeschen, C. (1985). Agrammatism versus paragrammatism: A fic-
titious opposition. In M. Kean (Ed.), Agrammatism (pp. 207–248).
Cambridge, MA: Academic Press.
Heeschen, C., & Kolk, H. (1988). Agrammatism and paragramma-
tism. Aphasiology, 2(3–4), 299–302.
Idsardi, W., & Raimy, E. (2013). Three types of linearization and the
temporal aspects of speech. In M. T. Biberauer, & I. Roberts
(Eds.), Challenges to linearization (pp. 31–56). Berlin, Germany:
Mouton de Gruyter.
Kean, M. L. (Ed.). (1985). Agrammatism. Cambridge, MA:
Academic Press.
Kertesz, A. (2007). Western Aphasia Battery (Revised). Boston, MA:
Pearson.
Kleist, K. (1914). Aphasie und geisteskrankheit [Aphasia and mental
illness]. Münchener Medizinische Wochenschrift, 61, 8–12.
Kolk, H., & Heeschen, C. (1992). Agrammatism, paragrammatism
and the management of language. Language and Cognitive
Processes, 7(2), 89–129.
Lewis, R. L., & Vasishth, S. (2005). An activation-based model of
sentence processing as skilled memory retrieval. Cognitive
S c i e n c e , 2 9 ( 3 ) , 3 7 5 – 4 1 9 . h t t p s : / / d o i . o r g / 1 0 . 1 2 0 7 /
s15516709cog0000_25
MacWhinney, B. (2000). The CHILDES project: Tools for analysing
talk (3rd ed.), Mahwah, NJ: Erlbaum.
MacWhinney, B., Fromm, D., Forbes, M., & Holland, A. (2011).
AphasiaBank: Methods for studying discourse. Aphasiology,
25(11), 1286–1307. https://doi.org/10.1080/02687038.2011.
589893
Magnusdottir, S., Fillmore, P., den Ouden, D.-B., Hjaltason, H.,
Rorden, C., Kjartansson, O., … Fridriksson, J. (2013). Damage
to left anterior temporal cortex predicts impairment of complex
syntactic processing: A lesion-symptom mapping study: ATL
damage impairs complex syntax processing. Human Brain
Mapping, 34(10), 2715–2723. https://doi.org/10.1002/hbm.22096
Matchin, W. G. (2018). A neuronal retuning hypothesis of sentence-
specificity in Broca’s area. Psychonomic Bulletin & Review, 25(5),
1682–1694. https://doi.org/10.3758/s13423-017-1377-6
Matchin, W., Hammerly, C., & Lau, E. (2017). The role of the IFG
and pSTS in syntactic prediction: Evidence from a parametric
study of hierarchical structure in fMRI. Cortex, 88, 106–123.
https://doi.org/10.1016/j.cortex.2016.12.010
Matchin, W., & Hickok, G. (2019). The cortical organization of
syntax. Cerebral Cortex, 30(8), 1–18.
Ogar, J. M., Baldo, J. V., Wilson, S. M., Brambati, S. M., Miller, B. L.,
Dronkers, N. F., & Gorno-Tempini, M. L. (2011). Semantic demen-
tia and persisting Wernicke’s aphasia: Linguistic and anatomical
profiles. Brain and Language, 117(1), 28–33. https://doi.org/
10.1016/j.bandl.2010.11.004
Pallier, C., Devauchelle, A.-D., & Dehaene, S. (2011). Cortical rep-
resentation of the constituent structure of sentences. Proceedings
of the National Academy of Sciences, 108(6), 2522–2527.
https://doi.org/10.1073/pnas.1018711108
Pillay, S. B., Binder, J. R., Humphries, C., Gross, W. L., & Book, D. S.
(2017). Lesion localization of speech comprehension deficits in
chronic aphasia. Neurology, 88(10), 970–975. https://doi.org/
10.1212/ WNL.0000000000003683
Rogalsky, C., & Hickok, G. (2011). The role of Broca’s area in sen-
tence comprehension. Journal of Cognitive Neuroscence, 23(7),
1664–1680.
Rogalsky, C., LaCroix, A. N., Chen, K.-H., Anderson, S. W.,
Damasio, H., Love, T., & Hickok, G. (2018). The neurobiology
of agrammatic sentence comprehension: A lesion study. Journal
of Cognitive Neuroscience, 30(2), 234–255. https://doi.org/
10.1162/jocn_a_01200
Saffran, E. M., Berndt, R. S., & Schwartz, M. F. (1989). The quanti-
tative analysis of agrammatic production: Procedure and data.
Brain and Language, 37(3), 440–479. https://doi.org/10.1016/
0093-934X(89)90030-8
Sapolsky, D., Bakkour, A., Negreira, A., Nalipinski, P., Weintraub,
S., Mesulam, M. M., … Dickerson, B. C. (2010). Cortical neuro-
anatomic correlates of symptom severity in primary progressive
aphasia. Neurology, 75, 358–366.
Schwartz, M. F., Saffran, E. M., & Marin, O. S. (1980). The word
order problem in agrammatism: I. Comprehension. Brain and
Language, 10(2), 249–262.
Thompson, C. K., Lange, K. L., Schneider, S. L., & Shapiro, L. P. (1997).
Agrammatic and non- brain-damaged subjects’ verb and verb argu-
ment structure production. Aphasiology, 11(4–5), 473–490.
Thothathiri, M., Kimberg, D. Y., & Schwartz, M. F. (2012). The neu-
ral basis of reversible sentence comprehension: Evidence from
voxel-based lesion symptom mapping in aphasia. Journal of
Cognitive Neuroscience, 24(1), 212–222. https://doi.org/
10.1162/jocn_a_00118
Tyler, L. K., Marslen-Wilson, W. D., Randall, B., Wright, P.,
Devereux, B. J., Zhuang, J., … Stamatakis, E. A. (2011). Left in-
ferior frontal cortex and syntax: Function, structure and behav-
iour in patients with left hemisphere damage. Brain, 134(2),
415–431. https://doi.org/10.1093/brain/awq369
Wilson, S. M. (2017). Lesion-symptom mapping in the study of spo-
ken language understanding. Language, Cognition and
Neuroscience, 32(7), 891–899.
Wilson, S. M., Eriksson, D. K., Schneck, S. M., & Lucanie, J. M.
(2018). A quick aphasia battery for efficient, reliable, and
Neurobiology of Language
224
l
D
o
w
n
o
a
d
e
d
f
r
o
m
h
t
t
p
:
/
/
d
i
r
e
c
t
.
m
i
t
.
e
d
u
n
o
/
l
/
l
a
r
t
i
c
e
-
p
d
f
/
/
/
/
1
2
2
0
8
1
8
6
7
6
9
6
n
o
_
a
_
0
0
0
1
0
p
d
/
.
l
f
b
y
g
u
e
s
t
t
o
n
0
7
S
e
p
e
m
b
e
r
2
0
2
3
Agrammatism and paragrammatism
multidimensional assessment of language function. PLOS ONE,
13(2), e0192773. https://doi.org/10.1371/journal.pone.0192773
Wilson, S. M., Henry, M. L., Besbris, M., Ogar, J. M., Dronkers,
N. F., Jarrold, W., … Gorno-Tempini, M. L. (2010). Connected
speech production in three variants of primary progressive
aphasia. Brain, 133(7), 2069–2088. https://doi.org/10.1093/
brain/awq129
Wilson, S. M., & Saygın, A. P. (2004). Grammaticality judgment
in aphasia: Deficits are not specific to syntactic structures,
Journal of Cognitive
aphasic syndromes, or lesion sites.
Neuroscience, 16(2), 238–252. https://doi.org/10.1162/
089892904322984535
Wilson, S. M., Yen, M., & Eriksson, D. K. (2018). An adaptive se-
mantic matching paradigm for reliable and valid language map-
ping in individuals with aphasia. Human Brain Mapping, 39(8),
3285–3307. https://doi.org/10.1002/hbm.24077
Yagata, S. A., Yen, M., McCarron, A., Bautista, A., Lamair-Orosco,
G., & Wilson, S. M. (2017). Rapid recovery from aphasia after
infarction of Wernicke’s area. Aphasiology, 31(8), 951–980.
https://doi.org/10.1080/02687038.2016.1225276
Yourganov, G., Smith, K. G., Fridriksson, J., & Rorden, C. (2015).
Predicting aphasia type from brain damage measured with struc-
tural MRI. Cortex, 73, 203–215. https://doi.org/10.1016/j.
cortex.2015.09.005
l
D
o
w
n
o
a
d
e
d
f
r
o
m
h
t
t
p
:
/
/
d
i
r
e
c
t
.
m
i
t
.
e
d
u
n
o
/
l
/
l
a
r
t
i
c
e
-
p
d
f
/
/
/
/
1
2
2
0
8
1
8
6
7
6
9
6
n
o
_
a
_
0
0
0
1
0
p
d
/
.
l
f
b
y
g
u
e
s
t
t
o
n
0
7
S
e
p
e
m
b
e
r
2
0
2
3
Neurobiology of Language
225